Bovine spongiform encephalopathy (BSE), commonly known as mad cow disease, is a progressive neurological pathology that affects cattle. The disease emerged in the 1980s, causing worldwide concern because of its potential transmission to humans through the consumption of contaminated products. BSE belongs to a group of neurodegenerative diseases known as transmissible spongiform encephalopathies (TSEs). These are characterised by the abnormal accumulation of an abnormal form of protein called a prion in the brain. These abnormalities then lead to distinctive brain lesions.
What is the pathogen?
Bovine spongiform encephalopathy (BSE), commonly known as mad cow disease, is a neurodegenerative disorder of the central nervous system of cattle. A specific type of molecular infectious agent, known as a prion or non-conventional transmissible agent (NCTA), causes the disease. In humans, it is known as variant Creutzfeldt-Jakob disease (vCJD).
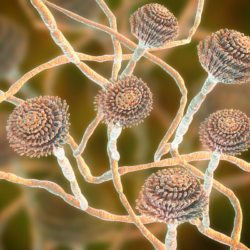
Prions are proteins consisting of an abnormal form of the PrP protein. In the case of TSEs, this abnormal form can spread throughout the body, mainly in the central nervous system. It then transmits its abnormality to other PrP molecules.
The exact nature of the BSE infectious agent is still debated, but the predominant theory supports the role of the prion. This protein, when it adopts an abnormal conformation, becomes resistant to proteases and accumulates in brain cells, causing them to degenerate.
TSEs, including BSE, are fatal neurodegenerative diseases affecting various animal species, including humans. Unfortunately, there is currently no treatment for these diseases. Prions are known to be resistant to conventional treatments such as heat and irradiation.
Because of the resistant and persistent nature of prions, the prevention and control of BSE involves strict biosecurity and surveillance measures in cattle populations to reduce the risk of transmission to humans and safeguard public health.
What does the disease look like in animals?
The BSE prion can infect mainly cattle. A few extremely rare cases of infection have been observed in cats. Transmissions to wild animals (ruminants and felids) in zoos have also been recorded.
The BSE prion is transmitted through the ingestion of contaminated meat and bone meal. However, animal meal has been banned in cattle feed since 1990, in ruminant feed since 1994, and in all animal feed since 2000. It is important to note that the disease is not transmitted from a living sick animal to a healthy one.
The symptoms of BSE are characterised by degenerative damage to the central nervous system after a very long incubation period. They include a deterioration in general condition, behavioural abnormalities such as hyper-sensitivity and exacerbated reactions, and motor coordination disorders that can lead to total paralysis.
Pathologically,BSE affects the brain and spinal cord of cattle. It causes lesions in the brain that can be seen under an optical microscope, including spongy changes and loss of neurons. External symptoms generally appear after an incubation period of around 4 to 5 years, in animals aged over 2 years. They may include behavioural changes, locomotor disorders and a reduction in milk production.
The diagnosis ofBSE is generally made after the death of the animal, by histopathological examination or a Western blot test on a fragment of the brain stem.
Unfortunately, there is no effective treatment for BSE. Affected animals will inevitably die if the disease continues.
How is bovine spongiform encephalopathy transmitted?
Mad cow disease is a zoonosis, meaning that it can only be transmitted to humans through food. When humans consume contaminated beef, they contract the human variant of mad cow disease. It is also known as variant Creutzfeldt-Jakob disease (vCJD). However, it is essential to stress that this disease is not contagious from one individual to another, either between humans or between humans and infected animals.
The incubation period for these diseases is long. It can sometimes take several years before symptoms appear. Once symptoms appear, they tend to worsen rapidly. Death usually occurs within two years.
Measures taken to prevent the spread of the disease include the ban on animal meal in the herbivore food chain since 1990. Specified risk organs (SRMs) have also had to be systematically removed from cattle at the abattoir and incinerated since 1996. These organs include the brain, eyes, tonsils, spinal cord, spinal column and part of the intestines.
It is important to note that no cases of occupational origin have been identified to date. On the other hand, certain professional activities expose workers to the risk of SRM contamination. These include slaughterhouse staff, cleaning and maintenance teams, rendering staff and veterinary laboratory staff.
This human form of mad cow disease, although similar to classical CJD, has a number of clinical and anatomical differences.
Although certain studies have confirmed the transmission of the bovine disease to humans, the exact means of transmission remains unknown. In addition, the disease has been transmitted by blood transfusion in exceptional cases.
Creutzfeldt-Jakob disease: symptoms in humans
There is a form of transmissible spongiform encephalopathy (TSE) specific to humans. It is known as Creutzfeldt-Jakob disease (CJD ). It is characterised by the accumulation of a prion in the central nervous system. The incubation period can last years or even decades before the onset of balance and sensitivity disorders and, eventually, dementia. The outcome is inevitably fatal, usually occurring within a year or so. The disease has various origins: most cases are sporadic, of unknown origin. It can also be hereditary (10% of cases).
Infection may be iatrogenic, resulting from medical procedures such as the use of hormones or brain tissue transplants, or from the use of inadequately decontaminated surgical instruments. CJD is the human equivalent of mad cow disease. CJD manifests itself through a variety of symptoms, including motor, cognitive, psychiatric, visual and cerebellar disorders. Its course is rapid and often fatal.
Variant Creutzfeldt-Jakob disease (vCJD)
Variant Creutzfeldt-Jakob disease (vCJD) is a rare acquired form of the disease. Most cases have been observed in the United Kingdom, with 178 cases recorded as of 7 May 2022. On the same date, 55 cases were reported in other European and non-European countries. VCJD develops after eating beef contaminated with bovine spongiform encephalopathy, or mad cow disease.
This form of the disease is characterised by symptoms appearing at a younger average age (under 30) than the sporadic form. The incubation period can vary from 12 to over 20 years. Four cases of vCJD were associated with blood transfusions between 1996 and 1999. The estimated prevalence in the UK is one carrier for every 2,000 people.
Although no cases of vCJD have been reported in North America, cases of bovine spongiform encephalopathy have been identified in the region. VCJD is characterised by neurological and psychiatric symptoms. It progresses slowly, over a median period of 14 months. Initial symptoms include neuropsychiatric disorders followed by progressive motor and cognitive deficits. Transmission to humans occurs through the consumption of contaminated meat. The infectious prion then spreads through the lymphoid tissues of the intestines before reaching the central nervous system. The parameters of infection, such as the infectious dose and incubation period, are still poorly understood.
Other forms
Creutzfeldt-Jakob disease (CJD) is the main prion disease in humans, characterised by several forms and subtypes. Symptoms include dementia, myoclonus and other central nervous system deficits. Death generally occurs within 4 months to 2 years, depending on the form and subtype of the disease. Treatment is mainly supportive.
The typology of the disease has several origins:
- The sporadic form, the most common, whose origin is unknown and not epidemic.
- The familial form, which accounts for around 5-15% of cases and is generally inherited in an autosomal dominant fashion. It is characterised by an early onset and potentially longer duration.
- The acquired form, which probably accounts for less than 1% of cases, results from the ingestion of prion-contaminated meat (variant Creutzfeldt-Jakob disease [vCJD]). It can also be contracted iatrogenically through medical interventions such as tissue transplants.
The most common symptoms include dementia,ataxia, myoclonus and visual disturbances. In the case of vCJD, psychiatric symptoms predominate rather than memory loss.
Despite the rarity of acquired disease, cases of iCJD have been reported following procedures such as tissue transplants or the use of products derived from the human body. Around 70% of CJD patients initially present with memory loss and confusion. A further 15-20% show incoordination of movement and myoclonus.
In addition to the characteristic symptoms, other neurological abnormalities such as hallucinations, convulsions and visual disturbances are frequently observed, particularly in sporadic cases of the disease.
Diagnosis
Levels of tau protein and neurofilament light chains in the blood increase significantly and correlate with the progression of the disease. This increase can be detected even before the first symptoms appear. In addition, testing for prion protein in the blood is a screening option.
Detection of the prion protein in various tissues is also possible using a technique called RT-QuIC (Real Time Induced Conversion). This has very high sensitivity and specificity.
The electroencephalogram (EEG) can reveal an abnormal trace with triphasic puffs and a slowing of the basic rhythm.Brain MRI reveals hypersignals in the cortical and/or basal ganglia, which are fairly specific signs. Lumbar puncture may reveal the presence of 14-3-3 protein and tau. However, these molecules do not appear to be directly involved in the disease, but are indicative of neuronal destruction.
Diagnosis can be complex. However, non-invasive tests such as diffusion-weighted MRI and RT-QuIC on cerebrospinal fluid offer valuable help in the early diagnosis of Creutzfeldt-Jakob disease.
How is this disease treated?
Unfortunately, no effective treatment or vaccine is available for any type of Creutzfeldt-Jakob disease. Doctors can only prescribe opiates to relieve pain, muscle relaxants and anti-epileptic drugs to reduce muscle stiffness and uncontrollable jerky movements.
The prognosis for Creutzfeldt-Jakob disease is generally poor, with death occurring within 6 to 12 months of the onset of the disease, often due to complications such as pneumonia. However, in the case of variant Creutzfeldt-Jakob disease, life expectancy appears to be slightly prolonged, with an average of around 1.5 years.
In terms of treatment, only supportive care is available to manage the symptoms associated with Creutzfeldt-Jakob disease. There is no curative treatment to slow or halt the progression of the disease, and medical interventions are mainly aimed at improving the patient’s comfort and quality of life.
What can be done to prevent the disease?
General preventive measures against Creutzfeldt-Jakob disease include actions in both animals and humans.
In animals, the following measures are essential:
- A ban on feeding meat and bone meal to all farm animals.
- Destruction by incineration of all animal carcasses and specified risk materials.
- Systematic screening for bovine spongiform encephalopathy (BSE) of all cattle over two years old presented for slaughter or rendering.
For humans, rigorous hygiene practices are essential:
- Cleaning and disinfecting premises and equipment in accordance with official health recommendations.
- Storage of waste and animal carcasses in dedicated refrigerated containers.
- Training and informing workers about the risks associated with BSE and the preventive measures to be taken.
In addition, it is crucial to put in place appropriate means to guarantee the safety of workers, in particular by providing drinking water, soap, personal protective equipment (PPE) and a first aid kit. Separate lockers should be used to avoid cross-contamination of clothing.
For activities involving contact with specified or contaminated risk materials, additional measures should be taken, such as increased hygiene precautions and the wearing of PPE appropriate to the task.
For medical equipment, steam autoclaving or immersion in specific disinfectant solutions is recommended to ensure the elimination of pathogens. Conventional sterilisation methods may prove ineffective.
Finally, at regulatory level, continuous monitoring of BSE cases in animals is essential, accompanied by strict measures such as a ban on potentially contaminated food, the appropriate destruction of dead animals and animal products, and the identification of animals to enable effective monitoring and follow-up of suspected cases.
The fight against BSE
Measures to combat infection with bovine spongiform encephalopathy (BSE) are governed by the French Rural Code. They include specific actions to monitor and manage the disease.
The following measures are implemented to control the spread of BSE in animals:
- Surveillance of livestock, including animals, buildings, milk and milk products.
- Isolation of sick animals, with disinfection of farm premises and contaminated effluent.
- Euthanasia of infected animals and their offspring, and destruction of the cohort of animals born around the affected animal.
From an animal health point of view, BSE is considered to be a contagious disease. From a public health point of view, however, all forms of Creutzfeldt-Jakob disease (CJD) are notifiable. At present, Creutzfeldt-Jakob disease is not included in the tables of occupational diseases.
The prion responsible for BSE is classified in risk group 3 in terms of safety at work. In the event of injury at a workstation involving contact with specified risk materials (SRMs), it is imperative to report the incident to the occupational physician.
Since the 1990s, the French authorities have gradually introduced bans on the use of meat and bone meal in animal feed in order to restrict the spread of BSE. Despite the implementation of these measures, cases of BSE persist. This is explained by failings in the application of regulations and cross-contamination between animal feed chains.
At Community level, the main BSE management measures include the ban on processed animal proteins in animal feed, the removal of specified risk materials from carcasses, the monitoring of rapid BSE diagnostic tests on slaughtered animals, and the introduction of animal health measures in the event of the detection of cases of BSE or scrapie.
Some epidemiological data…
Creutzfeldt-Jakob disease (CJD) was first detected in the United Kingdom in 1986. Since 1992, the Institut national de la santé et de la recherche médicale (INSERM), in collaboration with the Institut de veille sanitaire (InVS) and other European agencies, has overseen an epidemiological surveillance network for CJD. Despite efforts to prevent bovine spongiform encephalopathy(BSE), cases of CJD persist. Although epidemiological data show a decline in cases in recent years, the disease is still present.
For example, most cases of variant CJD have been recorded in the UK, with 178 cases up to May 2022, and only 2 since 2011. In addition, 55 cases were recorded in other European and non-European countries at the same date.
The last French case of CJD, a variant of the disease, was in 2019. However, fewer than 250 cases of CJD have been reported worldwide, mainly in the United Kingdom, following exposure of the human population to the agent responsible for BSE.
Animal health
Bovine Spongiform Encephalopathy (BSE) was first identified in the UK in 1986. It reached a peak in 1992, with 37,280 cases recorded that year. Although the epidemic has affected other European regions as well as certain foreign countries such as Japan, the United States and Canada, its scale remains smaller than that observed in the United Kingdom. Epidemiological studies quickly identified contamination by meat-and-bone meal used in cattle feed as a means of transmitting the pathogen.
Between 1986 and 2004, BSE was considered to be caused by a single agent, with the biochemical signature of the prion identical in all cases. However, in 2004, the appearance of two new biochemical profiles gave rise to what is now known as atypical BSE. Data on the distribution of this prion in tissues and on the epidemiology of these forms remains limited. The sporadic occurrence of these cases suggests that they may be spontaneous. Contaminated animal meal has also exposed small ruminants, causing a case of CJD in a goat in France in 2005. Despite increased surveillance measures, no other cases have been detected.
Other forms of Transmissible Spongiform Encephalopathy (TSE) have emerged, notably in mink and cats, following the transmission of the BSE agent via food. Since 2016, recent cases of chronic wasting disease have been reported in certain cervids in Northern Europe. In addition, a new TSE was identified in dromedaries in Algeria and Tunisia in 2018.
European experts have classified countries according to the risk of spreading BSE in their cattle herds. France is classified as a low-risk country. BSE surveillance in France has been based on three epidemiological surveillance programmes since 1991. It uses epidemiological surveys, systematic screening tests on animals at risk, and post-mortem analyses to detect the presence of BSE.
Human health
In France, since 1992, the Institut national de la santé et de la recherche médicale (INSERM), in collaboration with the Institut de veille sanitaire (InVS ) and their European partners, has overseen an epidemiological surveillance network for Creutzfeldt-Jakob disease (CJD).
Between 1992 and 2019, a total of 28 cases of definite or probable variant CJD (vCJD) have been identified in France, all of which resulted in the death of patients. These cases of vCJD have the following characteristics:
- 12 men and 16 women were affected.
- The median age at death or diagnosis was 36 years. Ages ranged from 19 to 58.
- 9 patients lived in the Île-de-France region and 19 in other regions.
Among the 26 cases of vCJD, deaths were recorded in different years, including 1996, 2000, 2001, 2002, 2004, 2005, 2006, 2007, 2009, 2013, 2014 and 2019. None had known risk factors for other forms of CJD. In addition, one case had been a regular visitor to the UK for around ten years from 1987.
In 2012, there were around 170 cases of vCJD in the UK and 50 cases in the rest of the world. Since 2000, the disease has become less common, with a typical age of onset of less than 30 years.
In France, the Réseau National de Surveillance de la MCJ (RNS-MCJ) receives all suspected cases of CJD, with over 1,000 notifications each year. Around 10% are confirmed as probable or definite cases.
The Agence nationale de santé publique, which took over from the InVS in 2016, publishes a table listing all reported cases of probable or definite CJD. This table, which is updated regularly, shows that the last update was on 31 January 2020. In the laboratory, tacrolimus and astemizole have been identified in vitro as potential antiprion agents in humans.
Mad cow crisis
The socio-economic crisis triggered by the emergence of bovine spongiform encephalopathy (BSE) profoundly affected society and the economy. As soon as public opinion became aware of the situation, a violent social crisis erupted. It was characterised by a glaring discrepancy between consumer expectations and farmers’ practices. Farmers feeding their cows with food supplements of various origins, notably mineral, synthetic or animal-based, aroused widespread suspicion. This has led to a drastic fall in beef consumption. This situation has plunged the sector into an economic crisis.
The media played a key role in amplifying the crisis. From the end of 1995, the British media reported growing concern about unexplained cases of Creutzfeldt-Jakob disease. They warned against eating beef. This media coverage heightened public concern. It also revealed a desire to lift the silence surrounding the problem. The media covered the story extensively, contributing to collective awareness and the scale of the social crisis.
The economic crisis has been particularly damaging to the French beef industry. The fall in beef consumption has led to a drop in prices and exports, putting farmers at risk. Faced with this situation, the French government has put in place various support measures, such as deferrals of social security contributions, subsidised loans and restructuring funds, to help those involved in the industry get through this difficult period.
At the same time, trade embargoes imposed on certain countries, notably the United Kingdom and the United States, have had a major impact on beef exports. This has exacerbated the international economic crisis.
Finally, the crisis has raised ethical and philosophical questions. These include the treatment of animals and feeding practices. The negative reactions observed in certain cultures, such as Hinduism, underline the importance of religious beliefs and perceptions of human nature in understanding these events.