Rosacea is a common dermatological condition affecting millions of people worldwide . This skin condition is characterised by redness, dilated blood vessels and pimples on the face, which can cause pain, discomfort and social embarrassment. Although rosacea is not a serious condition, it can have a significant impact on the quality of life of those who suffer from it. In this article, we’ll take a closer look at the causes, symptoms and treatment options for rosacea, a multifaceted skin condition.
What is rosacea?
Rosacea is a chronic inflammatory skin disease that alternates between periods of crisis and lulls. It is mainly characterised by diffuse redness in the centre of the face. Symptoms can vary from person to person: papules and pustules, thickening of the skin and various burning-type pains (tingling, tightness & paresthesias). People with rosacea also have a defective hydrolipidic skin barrier. As a result, they become hypersensitive to various everyday stimuli.
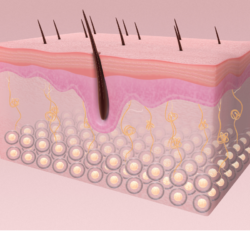
What is the skin?
The skin is made up of three layers: the epidermis or stratified epithelial tissue, the dermis or connective tissue and the adipose connective tissue, the hypodermis. It forms the body’s protective envelope, with three main functions:
- Protection from the outside world: preventing UV rays, allergens and pollution from entering the body
- A secretory role: Human skin has around 2,000,000 sebaceous glands, with a density of around 400 to 900 per square centimetre on the face. These glands, located in the dermis, secrete sebum. The role of sebum is to protect the skin from external aggression (thanks in particular to its antibacterial properties) and from dehydration (by preventing the water present in the tissues from evaporating).
- An ” absorbent ” function: the hypodermis is capable of absorbing shocks to the skin.
How is rosacea-sensitised skin characterised?
Atopic skin suffering from rosacea is considered hypersensitive and hyper-reactive: this is because the hydrolipidic film (composed mainly of water, sweat and sebum) no longer fulfils its protective role. When the skin barrier is compromised, the skin’s tolerance threshold is lowered. The result is exaggerated reactivity to internal and external aggression. Deregulation of the immune response, the vascular & neurological system and disruption of the balance of the skin barrier: a sensation of permanent discomfort, known as “rosacea”.
What are the visible symptoms of rosacea?
Rosacea can take many different forms, so it’s important to consult a dermatologist to establish a diagnosis & obtain appropriate treatment. Various symptoms can be attributed to this dermatosis, including the following:
- Persistent redness of the face, which may vary in intensity and location depending on the individual
- Thickening of the skin
- Oedema
- Visible blood vessels or telangiectasias
- Flushing or erythrosis
- Papules & pustules
- Nose deformity
- Desquamation of the epidermis
- Eye redness
The physical sensations that accompany it
The symptoms of rosacea are not necessarily visible. As a result, the dermatologist’s examination is essential. Here is the list of symptoms:
- Warmth, sensations of heat
- Tingling
- Tingling
- Paraesthesia
- Dryness/ severe eye discomfort
The impact of the disease on daily life
Rosacea also has a major impact on everyday life. It is true that this disease is not simply a “reddening” of the face. In fact, a survey carried out by the National Rosacea Society shows that almost 90% of rosacea sufferers believe that their skin condition has also contributed to a drop in their self-confidence. 41% of those questioned admit to avoiding all social interaction, while 88% are affected in their professional life. Finally, almost 51% had already been absent from work because of their rosacea.
Potential triggers of rosacea
- UV rays
- Sudden temperature changes
- Stress
- Intense sport
- Ingestion of very hot drinks or food
- Strong wind
- Spices
- Certain cosmetic products (e.g. alcohol, witch hazel, essential oils, flower extracts, perfume, cosmetic actives such as AHAs, benzoyl peroxide, etc.)
- Overwork
- Cold
- Sun
- Air conditioning
- Humidity
- Hormonal fluctuations
Progress in understanding the pathogenesis of rosacea
Recent research (6) has led to a better understanding of certain key mechanisms involved in the development of rosacea, thereby enriching our knowledge of this complex dermatological condition. Three major advances deserve particular attention: the involvement of the LL-37 protein (belonging to the cathelicidin family), the activity of TRP channels (potential transient receptors), and problems linked to the skin’s protective barrier.
- Role of the LL-37 protein: Cathelicidin, and more specifically the LL-37 protein, plays a critical role in rosacea. Normally, this protein helps fight infection by acting as an antimicrobial. However, in rosacea, excessive production or dysfunction of LL-37 can lead to inflammation and redness. A better understanding of this mechanism may lead to more targeted treatments to control this overreaction.
- Importance of TRP channels: TRP channels, present in skin cells, play a role in the perception of sensations such as heat or pain. In rosacea, abnormal activity of these channels can cause burning sensations and contribute to skin irritation and redness. This discovery helps us to understand why some rosacea sufferers experience increased sensitivity.
- Skin Barrier Dysfunction: Rosacea is often associated with a weakened skin barrier, which makes the skin more vulnerable to external irritants and promotes moisture loss. Research shows a link between this fragility of the skin barrier and increased activity of the STAT3 transcription factor in skin cells. This link suggests that strengthening the skin barrier could be a key strategy in the treatment of rosacea.
These advances offer promising prospects for the development of more appropriate and effective treatments for rosacea, by precisely targeting the underlying causes of the disease. By integrating these discoveries into our overall understanding of rosacea, we can propose more personalised therapeutic approaches aimed at alleviating not only the symptoms, but also the underlying causes of the condition.
Current drug treatments for rosacea
The management of rosacea has evolved over time, now offering a wide range of medicinal treatments. These treatments vary according to the severity and type of rosacea. Here is an overview of the main treatment options (6):
Topical treatments :
- Metronidazole: An antibiotic that reduces inflammation and erythema.
- Ivermectin: Effective against inflammation and itching, and also targets Demodex mites.
- Azelaic acid: Reduces inflammation and helps clear pores.
- Sodium Sulphacetamide / Sulphur: A mixture with antibacterial and keratolytic effects.
- Oxymetazoline and Brimonidine: Alpha-adrenergic receptor agonists, effectively reducing erythema.
- Adapalene: Although mainly known for its use in the treatment of acne, it may also be considered in certain specific cases of papulo-pustular rosacea. It is always advisable to consult a dermatologist for a personalised assessment and an appropriate treatment plan.
Oral treatments :
- Antibiotics Tetracyclines (such as Doxycycline and Minocycline): Used for their anti-inflammatory properties, particularly in papulopustular rosacea.
- Isotretinoin: Used in severe cases of rosacea, reduces sebum production and inflammation.
Off-label agents :
- Carvedilol: A beta-blocker that can help reduce redness and erythema.
- Hydroxychloroquine: Used to reduce mast cell infiltration and skin inflammation.
JAK/STAT inhibitors:
- Tofacitinib: A JAK inhibitor that has shown promising efficacy in reducing erythema.
Treatments targeting mast cells and microparticles:
- Tricyclic antidepressants and Acid Sphingomyelinase (aSMAse) inhibitors: Potentially useful in reducing inflammation and erythema by modulating microparticles.
Laser and light therapies :
- Used to treat redness, erythema and visible blood vessels.
A personalised approach to treating rosacea
The diversity of manifestations of rosacea means that the treatment of this skin condition cannot be uniform. Each patient presents a unique set of symptoms and reactions, requiring a personalised approach in the choice of therapies.
Adapting to different Rosacea phenotypes: Rosacea can manifest itself in a variety of forms, from simple erythema to inflammatory pustules and eye problems. Each type of rosacea requires specific treatments, and what works for one patient may not be effective for another. For example, topical treatments may be sufficient for mild rosacea, while more severe forms may require a combination of oral medication and laser therapy.
Consideration of Individual Response: It is also crucial to understand that each individual responds differently to treatments. What may relieve symptoms quickly in one person may be less effective, or even cause side effects, in another. Regular monitoring and adjustment of treatment is therefore essential to find the most beneficial balance.
Dermatological consultation and follow-up: A dermatologist can play a decisive role in devising a suitable treatment plan. By carefully assessing symptoms, medical history and reactions to treatment, the specialist can adjust the therapeutic strategy to optimise effectiveness and minimise inconvenience.
Natural solutions to accompany conventional treatments
Discover a variety of natural remedies and gentle methods to effectively complement your medical treatment for rosacea.
Diet & lifestyle
It’s very important to pay attention to what you eat. Many foods and drinks can trigger rosacea attacks:
- Tomatoes
- Highly acidic foods (vinegar, lemon, etc.)
- Spices such as pepper, chilli, curry (cinnamon for some) and ginger
- Dark chocolate
- Alcohol
- Very hot drinks
- Very sweet foods
As you’ll have realised, skin health is closely linked to intestinal health, so dietary adjustment is essential to managing rosacea symptoms: take care of your liver by applying a hot water bottle to your stomach after your evening meal, and pamper your intestines by facilitating transit through fibre-rich foods. Take some time for yourself: find an activity that allows you to disconnect from your daily routine, to get rid of the excess stress (walking,grounding, writing orjournaling, drawing, etc.). Lack of sleep has a considerable impact on skin healing. To help it regenerate, it’s important to get a good night‘s sleep.
Supplements to accompany your anti-rosacea diet
- Depuragem from the Herbalgem laboratory
- Dermagem from the Herbalgem laboratory
- Fig bud from the Herbalgem laboratory
- Vitarscorbol vitamin C gummies
- Superdiet special circulation quartet
- Nat&Form cod liver oil capsules
- Nat&Form liposomal zinc
- Solaray brand magnesium citrate
- Superdiet burdock (check out Clémentine ‘s article on our blog!)
- Curcuma Pileje (check out our blog post on turmeric to find out about its benefits)
Routine for skin prone to atopy/rosacea
In the morning, after rinsing your face with lukewarm water (not too hot, not too cold: remember that rosacea doesn’t like sudden changes in temperature), choose a gentle cleanser to preserve the skin’s hydrolipidic film, like Cerave’s fragrance-free moisturising cleanser.
Bioderma Créaline anti-redness moisturiser should be applied to damp skin with the fingertips, followed by the same brand’s sun protection. You can also choose the organic neutral cream from Avril.
Vichy Normaderm is a non-comedogenic, covering, non-irritating foundation. However, if you’re a BB cream fan, Dermaceutic offers a tinted DD cream, available in two shades (a combination of BB cream and high sun protection + antioxidants to help with redness). Avène also offers a fluid foundation for sensitive rosacea skin.
In the evening, , it’s very important to cleanse the skin thoroughly to remove residues of sun protection, make-up and all the dirt accumulated during the day: choose a quality jojoba oil, and apply it to the entire face with a damp cotton pad before using the moisturising cleanser from Cerave. On damp skin, use Cicaplast soothing healing spray before applying your evening moisturiser, depending on your skin’s “daytime” needs: Créaline moisturiser AR or Cerave moisturising cream. Laroche-Posay Healing Accelerator Gel is an excellent alternative to Japanese-style Sleeping Packs as the last step in your routine, to seal in moisture and prevent trans-epidermal water loss during the night.
Optimise your rosacea care routine with Soin & Nature
Managing rosacea isn’t just about medical treatments. To effectively complement your skincare routine and maximise results, it’s essential to incorporate parapharmacy products specially designed to soothe, protect and repair the skin affected by this condition. Discover our selection of parapharmacy products that make a difference:
| Product | Use |
|---|---|
| Avene Anti-Redness Rosamed Concentrated Care | Treatment of skin redness, particularly for sensitive, reactive or intolerant skin. |
| SVR Sensifine AR Cream Spf50+ 50 ml | SPF50+ sun protection and soothing anti-redness care for skin prone to couperose. |
| ACM Azeane 15% Azelaic Acid Cream | Reduces inflammation, imperfections and redness, suitable for all skin types. |
| SVR B3 Hydra Repair Concentrate Ampoule | Moisturises dehydrated and sensitive skin, reduces redness and tightness. |
| Cicaplast Scar Repair Accelerator 40ml | Stimulates epidermal reconstruction for dry and dehydrated skin. |
| Avene Cicalfate+ Anti Scar Gel | Improves the appearance of recent scars, moisturises and protects the skin. |
These products, selected for their effectiveness and gentleness, are your allies in bringing comfort and well-being to your skin every day. Incorporate them into your skincare routine for soothed skin and a harmonised complexion.
Can witch hazel help with rosacea?
Witch hazel (Hamamelis virginiana) is often used in skin care products for its astringent, anti-inflammatory and haemostatic properties. However, it is not recommended for people with rosacea for a number of reasons.
Firstly, its astringent properties can cause excessive dryness and irritation. Secondly, witch hazel contains tannin, which can aggravate inflammation. Finally, some witch hazel products may contain alcohol, which is known to cause redness and inflammation. It’s advisable to consult a healthcare professional before adding a new ingredient to your skincare routine, especially if you have a skin condition such as rosacea.
Sources
- https://pubmed.ncbi.nlm.nih.gov/16029676/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048199/
- https://pubmed.ncbi.nlm.nih.gov/32199994/
- https://www.frontiersin.org/articles/10.3389/fmed.2023.1292722/full