The prostate is a gland that sometimes causes problems for men of a certain age. In fact, when it becomes diseased, it can be a source of various inconveniences. Among the problems it causes are urinary and erectile problems. It’s true that this situation is frightening, but it needn’t be taken for granted. Rest assured, there are ways of alleviating the problem. So, in the following paragraphs, discover the best treatment for the prostate.
A major public health issue in France
Before delving into the details of prostate cancer, it’s important to understand the scale of the disease in France. In 2023, prostate cancer is estimated to be the most common cancer in men, with 59,885 new cases. This represents a slight increase on the 59,800 cases recorded in 2018. This type of cancer accounts for around 25% of male cancers, with an annual incidence of 81 cases per 100,000 men. It is therefore a significant public health problem in France.
Although prostate cancer is the most common cancer in men, it is not the most deadly. Thanks to advances in screening and treatment, many cases are effectively treated, often by complete removal of the prostate. This information is crucial to understanding both the prevalence and treatment prospects for this disease.
Definition of prostate cancer
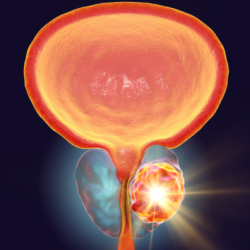
Prostate cancer is a type of cancer that develops in the cells of the prostate, a gland of the male reproductive system located below the bladder and in front of the rectum. This gland, about the size of a walnut in young men, produces some of the fluid that forms sperm. With age, the gland can change in size, becoming enlarged in older men.
This cancer is characterised by a malignant tumour formed by cancerous cells capable of invading and destroying neighbouring tissues. In some cases, it can also spread (metastasise) to other parts of the body. Prostate cancer is the most common cancer in men, particularly older men. There are variations in its prevalence according to ethnic origin: black men (of African and Caribbean descent) are more affected than white men, while men of Asian descent are less affected. Trans women and non-binary people assigned male at birth can also develop this type of cancer.
Prostate cancer generally develops slowly and can often be removed completely or managed effectively if diagnosed at an early stage. It is common for older men with this cancer to die of other causes. Adenocarcinoma is the most common type of prostate cancer, accounting for around 95% of all cases.
Types of prostate cancer
Adenocarcinoma, the most common type of prostate cancer, accounts for around 95% of all cases. It develops in the glandular cells of the prostate, which produce the prostatic fluid mixed with semen. Adenocarcinoma is often found in several places in the prostate, a condition known as multifocal cancer.
In addition to adenocarcinoma, there are rare types of prostate cancer tumours, including:
- Urothelial carcinoma, also known as transitional cell carcinoma.
- Sarcoma.
- Small cell carcinoma.
- Carcinoid tumours.
- Squamous cell carcinoma.
Each of these rare types has different characteristics and treatment methods. Knowing the specific nature of the cancer is crucial in determining the most appropriate treatment.
Pre-cancerous states of the prostate
In addition to prostate cancer, there are pre-cancerous conditions that can increase the risk of developing cancer. These conditions are not cancerous in themselves, but they can develop into cancer if left untreated or unmonitored:
- Prostatic Intraepithelial Neoplasia (PIN): This is a condition where abnormal changes occur in the epithelial cells that line the prostate glands. PIN can be classified as low-grade or high-grade. High-grade PIN increases the risk of prostate cancer.
- Proliferative Inflammatory Atrophy (PIA ): This term refers to areas of the prostate where cells are smaller than normal and inflamed. Although AIP is not cancerous, research suggests that there may be a link between AIP and high-grade PIN or prostate cancer.
- Atypical Small Acinar Proliferation (ASAP): This condition is characterised by abnormal growth of glandular cells in the prostate. Although not all men with ASAP develop prostate cancer, increased surveillance and follow-up biopsies are often recommended.
Monitoring these precancerous conditions is crucial for the prevention and early management of prostate cancer.
The prostate and the conditions that affect it
The prostate is a small gland located below the bladder in men. It produces part of the seminal fluid that carries sperm during ejaculation. Unfortunately, the prostate can be affected by a number of conditions that can cause unpleasant symptoms and impair quality of life. These conditions include benign prostatic hyperplasia (BPH), prostate cancer, inflammation of the prostate and urinary tract infections. In this section, we’ll explore the different conditions that can affect the prostate, their symptoms, causes and possible treatments.
Prostate enlargement
Benign prostatic hyperplasia, also known as prostate adenoma, is a common condition in men aged around 50. It is characterised by an increase in the size of the prostate gland, which can lead to symptoms such as pain when urinating, a frequent urge to urinate and an interruption or reduction in the strength of the urine stream. Although BPH is not prostate cancer, it can cause significant discomfort and affect quality of life. Treatments for BPH include medication, surgery and dietary supplements. It is important to consult a doctor to determine the best treatment for each specific case.
Prostatitis
Prostatitis is an inflammation of the prostate gland that affects men of all ages. It is generally caused by intestinal bacteria of the Escherichia coli type. Symptoms include burning sensations during urination and frequent urges to urinate. There is also pain in the penis and urethra. All these signs are often accompanied by fever, muscle pain and general malaise.
Prostate cancer
Prostate cancer is difficult to detect in its early stages. It presents no symptoms until the tumour swells. When this happens, the signs are similar to those of the two diseases mentioned above. The patient experiences incontinence, frequent urges to urinate and difficulty in passing urine. But apart from this, they also experience pain during ejaculation and erectile dysfunction. Traces of blood may even be found in his urine and semen.
Prostate treatments
When the pain and discomfort associated with the prostate worsen and become unbearable, specialists recommend surgery. But before this happens, there are products and medicines to relieve the symptoms of this disease. Most are available from chemists.
Food supplements
In addition to conventional treatments, dietary supplements can be taken to support prostate health. These supplements often contain natural ingredients and can help reduce inflammation, improve urinary function and prevent oxidative damage in the prostate. Although these supplements cannot cure prostate problems, they can be used alongside conventional treatments to improve results and reduce side effects. Here are some examples of dietary supplements for the prostate:
- Saw palmetto: also known as saw palmetto, saw palmetto is often used to treat the symptoms of BPH. Studies have shown that taking saw palmetto supplements can reduce BPH symptoms and improve urinary flow.
- Zinc: Zinc is an important mineral for prostate health. Studies have shown that men with prostate cancer often have lower than normal levels of zinc. Taking zinc supplements can help maintain normal levels of zinc in the body and support prostate health.
- Omega-3: Omega-3 fatty acids, found in oily fish such as salmon, can help reduce inflammation in the body and improve prostate health. Studies have shown that consuming omega-3s can reduce the risk of prostate cancer.
- Isoflavones: Isoflavones are plant compounds found in foods such as soya and beans. Studies have shown that isoflavones can help reduce BPH symptoms and support prostate health.
It’s important to talk to a doctor before you start taking prostate supplements, as some supplements can interact with other medicines or have unwanted side effects.
Diet and the prostate
Diet plays an important role in prostate health. Some studies have shown that certain foods can help prevent prostate problems, while others can increase the risk of prostate disease. Here are some foods to include or avoid to maintain a healthy prostate:
Foods to include
- Fruit and vegetables: Fruit and vegetables are rich in antioxidants and vitamins, which can help reduce inflammation and protect the prostate against oxidative damage. Cruciferous vegetables, such as broccoli and cauliflower, are particularly beneficial for prostate health.
- Healthy fats: healthy fats, such as the omega-3 fatty acids found in oily fish, can help reduce inflammation and improve prostate health.
- Green tea: Green tea contains compounds called catechins, which may help reduce the growth of prostate cancer cells.
Foods to avoid
- Processed foods: processed foods, rich in saturated fats and sugar, can increase inflammation in the body and increase the risk of prostate disease.
- Red meat: excessive consumption of red meat can increase the risk of prostate cancer. It is recommended that you limit your consumption of red meat in favour of lean meats such as chicken and fish.
- Dairy products: some studies have shown that excessive consumption of dairy products can increase the risk of prostate cancer. It is recommended that you limit your consumption of dairy products in favour of plant-based alternatives, such as almond or soya milk.
Here is a summary table of the recommended diet for prostate cancer, based on information from UCSF Health:
| Category | Recommendations | Notes |
|---|---|---|
| General Diet | Mainly plant-based, rich in fruit and vegetables, high in fibre, low in fat, limited in simple sugars | |
| Plant-based foods | Fruit and vegetables, wholegrain cereals, beans and pulses, other sources of vegetable protein | |
| Fruit and vegetables | Contain vitamins, minerals, fibre and anti-cancer phytochemicals | Eating at least 28 portions a week reduces the risk of prostate cancer |
| Fibre | Linked to reducing levels of hormones involved in the progression of prostate cancer | Aim for 25-35 grams of fibre a day |
| Low-fat diet | Aim for 20% of total calories from fat, with less than 10% saturated fat | |
| Simple sugars | Limit consumption of simple sugars | Avoid sweets, cookies, cakes and refined flour products |
| Liquids | Drink plenty of water | Necessary for a fibre-rich diet |
| Moderate calorie restriction | Reducing calorie intake can reduce the risk of various cancers |
These recommendations are specific to prostate cancer and may vary for other types of cancer.
The role of autophagy in prostate cancer
Autophagy, a complex and adaptable cellular process, plays a significant role in prostate cancer. This mechanism, often described as a phenomenon of ‘self-degradation’, enables cells to cope with metabolic, toxic and even infectious stress.
Autophagy and prostate cancer progression
Although autophagy is generally considered beneficial, it can also enhance nutrient utilisation and promote the growth characteristics of cancer cells. In advanced prostate cancer, preclinical evidence suggests that autophagy facilitates both disease progression and therapeutic resistance. Common therapies such as androgen deprivation, taxane-based chemotherapy, targeted kinase inhibition, and nutrient restriction can all induce significant cellular distress and, consequently, autophagy. (11)
Autophagy, apoptosis and disease progression
In prostate cancer, autophagy plays a pivotal role in regulating apoptosis and disease progression. Several molecular pathways are involved, notably PI3K/AKT/mTOR. However, depending on the cellular context, autophagy can play either a detrimental or protective role in prostate cancer. Current studies have investigated how autophagy interacts within these complex interactions, in particular to better understand the therapeutic response and resistance to chemotherapy in prostate cancer. (13)
Targeting autophagy in prostate cancer treatment
Attention has recently focused on the role of autophagy in cancer and how its modulation offers effective anti-cancer therapy. It has been shown that autophagy can promote or inhibit the proliferation and survival of prostate cancer cells. In addition, prostate cancer cell metastasis is affected (via induction and inhibition) by autophagy. Autophagy may affect the response of prostate cancer cells to therapies such as chemotherapy and radiotherapy, given the close association between autophagy and apoptosis. Increasing evidence has shown that upstream mediators such as AMPK, non-coding RNAs, KLF5, MTOR and others regulate autophagy in prostate cancer. (14)
Inhibition of autophagy and hormone therapy
A critical evaluation of the studies reviewed suggests that autophagy inhibition combined with androgen deprivation therapy is a promising approach for the treatment of prostate cancer. The regulatory effects of androgens on autophagy in prostate cancer cells are particularly discussed in order to highlight the effects of modulating autophagy during androgen deprivation. (11)
Alpha-blockers (alfuzosin, doxazosin, tamsulosin, terazosin…)
Alpha-blockers (alfuzosin, doxazosin, tamsulosin, terazosin, etc.) are drugs commonly used to treat benign prostatic hyperplasia. They work by relaxing the muscles of the bladder, urethra and prostate, which facilitates the flow of urine and relieves the symptoms of BPH. They can be taken alone or in combination with other medicines to improve the effectiveness of treatment.
5-alpha reductase inhibitors, such as tasteride or finasteride, are also used to treat BPH. These drugs work by blocking the production of a hormone called dihydrotestosterone, which stimulates prostate growth. By blocking this hormone, 5-alpha reductase inhibitors can reduce the size of the prostate and relieve the symptoms of BPH. However, they can take several months to show significant results and can cause side effects such as sexual problems. It is important to discuss with a doctor whether these drugs are suitable for your specific case.
Recent advances in the treatment of prostate cancer
This section presents the latest discoveries and innovations in the treatment of prostate cancer, providing an overview of pharmacological therapies, advanced diagnostic techniques and emerging therapeutic strategies that are transforming the management of this disease.
Innovative pharmacological treatments
Current standard treatments for prostate cancer include androgen deprivation therapy (ADT) in combination with androgen receptor targeting agents (ARTAs) or docetaxel chemotherapy. For pre-treated patients, new therapeutic options such as cabazitaxel, olaparib and rucaparib for BRCA mutations, Radium-223 for symptomatic bone metastases, sipuleucel T and 177 LuPSMA-617 are available, broadening the spectrum of effective treatments against various manifestations of the disease. (8)
New treatment options
Researchers at Cedars-Sinai Cancer have identified two new treatment options for men with recurrent prostate cancer. These treatments have shown superior efficacy to current standard therapy, prolonging progression-free survival while preserving quality of life. These discoveries, if approved by the Food and Drug Administration, could transform current prostate cancer treatment practices. (9)
Use of nanoparticles
Nanoparticles are being explored as an innovative means of targeting and delivering drugs specifically to prostate cancer cells. This approach could improve treatment efficacy while reducing side effects, offering a promising new strategy in the fight against prostate cancer. (10)
Improved biopsies
Traditionally, prostate cancer has been diagnosed by systematic biopsy, with needles inserted under transrectal ultrasound guidance. However, this method can miss high-grade cancers or identify low-grade cancers that do not require immediate treatment. To overcome these limitations, scientists at the NCI have developed a procedure combining magnetic resonance imaging (MRI) and transrectal ultrasound, enabling more accurate biopsies and better detection of high-grade prostate cancers.
Artificial intelligence in diagnostics
Artificial intelligence and machine learning are increasingly being used to improve prostate cancer diagnosis. These technologies help to better identify suspicious areas in MRI scans of the prostate that need to be biopsied, and assist pathologists in accurately assessing the grade of cancer, a key factor in determining the treatment required.
Imaging and WLPSM
Advanced imaging techniques targeting PSMA (prostate specific membrane antigen) are being developed to improve the diagnosis of recurrent prostate cancer. These techniques can detect tiny deposits of prostate cancer that would otherwise be undetectable, aiding more informed treatment decisions. Research from the NCI’s Cancer Moonshot℠ is also investigating the use of PSMA-PET to identify men at high risk of cancer recurrence.
New treatments for prostate cancer
Standard treatments for localised prostate cancer include surgery or radiotherapy, possibly combined with hormone therapy. An active surveillance option is also being considered for men with a low risk of disease progression. This approach involves regular monitoring of the cancer with biopsies and delaying treatment unless there are signs of disease progression.
Hormone therapy for prostate cancer
Several new approaches to hormone therapy for advanced or metastatic prostate cancer have been approved in recent years. Drugs such as enzalutamide, abiraterone, darolutamide and apalutamide have been shown to prolong survival in some men with castration-resistant prostate cancer.
PARP inhibitors for prostate cancer
PARP inhibitors, which block an enzyme involved in DNA repair, have become a treatment option for some men whose prostate cancer has genetic defects and has metastasised. Studies are underway to evaluate the combination of PARP inhibitors with hormonal therapies.
Vaccines for prostate cancer
Immunotherapies, which harness the power of the immune system to fight cancer, include treatment vaccines and immune checkpoint inhibitors. For example, sipuleucel-T is approved for men with little or no symptoms of metastatic CRPC.
Immunotherapy: Checkpoint inhibitors for prostate cancer
Immune checkpoint inhibitors, such as pembrolizumab and dostarlimab, are approved to treat tumours, including some prostate cancers, with specific genetic characteristics.
Targeted radiation therapy and WLPSM
Targeted therapies based on PSMA are being developed to treat advanced prostate cancer. Lu177-PSMA-617, recently approved by the FDA, has shown promising results in the treatment of certain types of metastatic prostate cancer.
Customised clinical trials for prostate cancer
Advances in our understanding of the genetic changes associated with prostate cancer are making it possible to propose personalised clinical trials based on the mutations found in the cancer, rather than its location in the body. These approaches could offer new therapeutic options for men with metastatic prostate cancer.
Source:
- https://www.vidal.fr/maladies/reins-voies-urinaires/hypertrophie-benigne-prostate-hbp/traitements.html
- https://www.cancer-environnement.fr/fiches/cancers/cancer-de-la-prostate/
- https://www.health.harvard.edu/topics/prostate-health
- https://cancer.ca/fr/cancer-information/cancer-types/prostate/what-is-prostate-cancer
- https://www.santepubliquefrance.fr/maladies-et-traumatismes/cancers
- https://www.alcimed.com/fr/les-articles-d-alcim/nouveau-traitement-cancer-prostate/
- https://pubmed.ncbi.nlm.nih.gov/36794353/
- https://www.sciencedaily.com/releases/2023/10/231018194545.htm
- https://www.cancer.gov/types/prostate/research
- https://pubmed.ncbi.nlm.nih.gov/25134829/
- https://jeccr.biomedcentral.com/articles/10.1186/s13046-022-02293-6
- https://pubmed.ncbi.nlm.nih.gov/35409187/
- https://pubmed.ncbi.nlm.nih.gov/35317831/