In winter, it is difficult for the body to synthesize vitamin D, which can lead to many health problems (depression, poor absorption of calcium and phosphate, increase in autoimmune diseases, etc.)
Insufficient exposure to sunlight predisposes to vitamin D deficiency. Deficiency induces disturbances in bone mineralization, leading to rickets in children and osteomalacia in adults and may contribute to osteoporosis. It is therefore advisable to do two cures per year: At the beginning of autumn and at the beginning of spring.
What is vitamin D?
Vitamin D or calciferol is fat soluble. It is also a hormone found in food and synthesized in the human body from a derivative of cholesterol under the action of UVB radiation from the Sun.
In humans, it exists in two forms:
- D2 (ergocalciferol) It is produced by plants.
- D3 (cholecalciferol) The latter is the natural form and the form used for low dose supplementation. It is of animal origin.
What is the difference between vitamin D2 and D3?
When our skin makes vitamin, it is called D3. Once ingested, all of vitamin D3 binds to a transport protein in the blood to be delivered to the liver. When it arrives in the liver, it undergoes a change in its chemical structure and gives a new form of calciferol (25 (OH) D3). It is this so-called “circulating” form that is measured when a blood sample is taken to find out its status.
It is from this circulating form that the active form is synthesized, according to the needs of the body. This is because in response to signals indicating a need, circulating vitamin D will undergo a further change in its chemical structure, which will take place mainly in the kidneys (but also in other cells).
D3 is better metabolized and thus leads to the active form of vitamin D more efficiently than D2.
Pharmacopoeias consider these steroid hormones to be equivalent and interchangeable. However, several studies show that D3 increases serum 25 – hydroxyvitamin D levels more effectively than vitamin D2. In particular, this has a lower plasma half-life and lower affinities for the vitamin D transporter protein and for its receptor.
What is the role of vitamin D and its metabolites?
| Organs | Action |
|
Immune system |
Stimulates immunogenic and anti-tumor activities Reduces the risk of autoimmune diseases |
| Intestine | Increases the transport of calcium and phosphorus (through better absorption) |
| Kidneys | Increases the reabsorption of calcium by the tubules |
| Parathyroid glands | Inhibits the secretion of parathyroid hormone |
| Pancreas | Stimulates the production of insulin |
| Bone | Promotes bone formation by maintaining proper concentrations of calcium and phosphate |
What are the effects of vitamin D on the immune system?
Vitamin D interferes in particular with our immune system, at different levels:
- It helps maintain the integrity of the intestinal mucosa, through its action on the proteins constituting the junctions between the intestinal cells:
Since the intestine is the place of transit for pathogens, their passage into the bloodstream can only be done by crossing the intestinal wall. When this wall is altered, it exhibits hyperpermeability which allows these pathogens to pass. A healthy gut wall is essential to prevent their passage, as is a diverse gut microbiota.
- It has an action on the innate immune system:
This dietary supplement stimulates macrophages and dendritic cells, which are the “front line soldiers” of the immune system. Our body reacts quickly in the event of an attack.
- It also stimulates the adaptive immune system:
By increasing the number of T lymphocytes, thus leading to an anti-inflammatory effect.
- It increases the pathogen elimination mechanisms:
Such as the synthesis of antimicrobial agents by immune cells.
- It has been widely studied in the context of the prevention of acute lung infections:
Vitamin D3 supplementation appears to reduce the risk of getting a respiratory tract infection at least once.
Vitamin D and Covid-19
Lack of vitamin D can be a risk factor for severe forms of Covid-19. However, it should not be taken without medical advice.
Its supplementation could reduce the risk of flu and COVID-19 infection.
It seems to promote the activation of the immune response and limit the harmful consequences of the pathogen-induced immune pathology. In the literature, there is evidence linking this vitamin deficiency on the one hand to susceptibility to acute viral infections and on the other hand to the more unfavorable course of certain chronic infections. This review examines current knowledge about vitamin D and its influence on the risk of respiratory infections (influenza epidemics and COVID-19 pandemic).
During the current coronavirus pandemic, several scientific publications, including a British study of 20 European countries, noted deficiencies in patients with COVID-19. Vitamin D deficiency has been found to increase the risk of severe disease or even death from coronavirus.
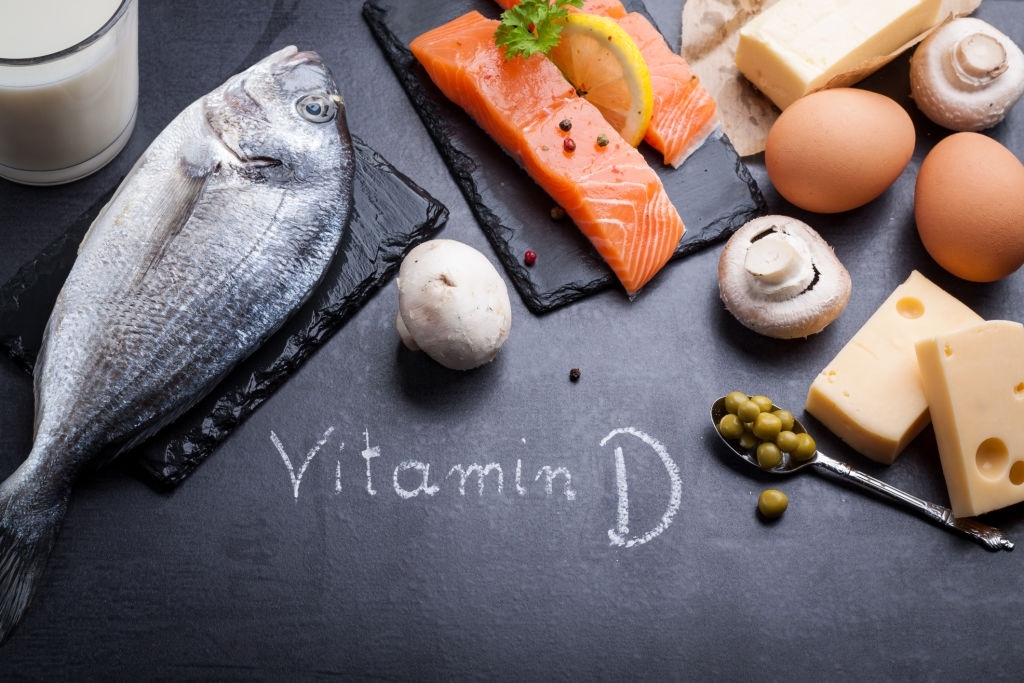
Vitamin D in the diet:
- The salmon
Fat-soluble vitamin D is found in significant amounts in the flesh of fatty fish. Smoked salmon cooked in the oven or steamed contains approximately 8.7 µg / 100g.
- Mackerel
Like all fatty fish, its lipids contain a majority of polyunsaturated fatty acids and in particular omega 3, endowed with beneficial effects on the cardiovascular system, and baked, it contains 7.72 µg of vitamin D per 100 g.
- Sardines
In summer, when the time has come for barbecues and meals in the garden, grilled sardines are a dish that always has its little success. And that is very good for our reserves of vitamin D, since it contains 10.8 µg per 100 g.
- Herring
Like mackerel and salmon, herring is one of these fatty fish, both rich in good fats (especially omega-3) and vitamin D. Smoked, it contains 22 µg per 100 g.
- Eel
Cooked, it contains 92 µg of vitamin D per 120 g.
- Anchovies
Raw, they provide enough to satisfy an adult’s daily intake of vitamin D in just a few bites! Indeed, anchovies contain 11 µg per 100 g.
- Cod liver oil
It is the richest food in vitamin D that exists. It contains 250 µg for 10 cl.